Episode 9: Sunday August 16
Drs. Sam Jejurikar, Dr. Salvatore Pacella, and Dr. Sam Rhee go through a breast augmentation case and discuss what to consider before, during and after your procedure.
They also talk about what is important to consider in choosing your size, as well as the hot-button topic breast implant illness.
Full Transcript (download the PDF)
S01E09 - 3 Plastic Surgeons and a MIcrophone - Breast Augmentation
Dr. Sam Rhee: [00:00:00] All right. And we are ready to go. This is Three Plastic Surgeons and a Microphone with as always the gentlemen, Dr. Sam Jejurikar out of Dallas, Texas, Instagram handle @samjejurikar, Dr. Salvatore Pacella. out of San Diego, LaJolla, California. His Ig handle is @sandiegoplasticsurgeon. And I am Dr. Sam Rhee from Paramus New Jersey and my Instagram handle is @bergencosmetic.
So welcome, gentlemen, how are you?
Dr. Sam Jejurikar: [00:00:29] Doing great. How about you gentlemen?
Dr. Salvatore Pacella: [00:00:32] Fantastic. Thank you. Good morning, everybody.
Dr. Sam Rhee: [00:00:35] All right. just remember this show is not a substitute for professional medical advice, diagnosis or treatment. This show is for informational purposes, only treatment and results may vary based on circumstances, situation, and medical judgment after appropriate discussion, always seek the advice of your surgeon or other qualified healthcare provider.
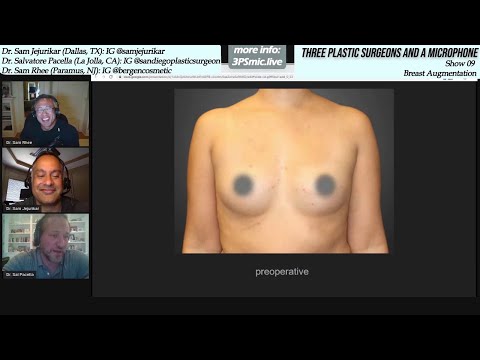
With any questions you may have regarding medical care. And never disregard professional medical advice or delay seeking advice because of something in this show. So this is going to be our breast augmentation show today. And I have a case from, a wonderful patient, who was very gracious to allow me to show her photographs and her results today.
And, let's get started.
So this is, so this is mainly a way that I thought, you know, you, I could hear both Sam and Sal, talk about their approach in terms of, breast augmentation, their thoughts when they, interact with their patients. And, and what they think is important for breast augmentation, obviously breast augmentation is one of the most popular procedures. It, I'm sorry. It's actually the most popular cosmetic surgical procedure in the U S for the past 10 years. with 313,000 patients alone in 2018, which is up 50% from 2000. and so as a result, obviously all plastic surgeons who do cosmetic surgery, have, generally speaking, have a fair amount of experience with breast augmentation.
So this was a patient of mine who, is in, you know, she's relatively young, no children and she just wished to have larger breasts. What are the main things that you guys think of when you have new patient consultations for breast augmentation?
Dr. Sam Jejurikar: [00:02:25] I'll, I'll start, you know, and, and I'm sure I'm going to touch on a lot of things that Sal and you would say.
So I think, plastic surgeons and patients approach breast augmentation slightly differently, patients oftentimes will come in and they sort of focus on cup sizes. I'm a, this cup and I want to be a two or three cup sizes, bigger. I want to be a D cup for instance, but I think we all, we look at a patient like this.
Think of, think about terms in terms of a dimensional analysis. So when I see this patient, you know, if you look at, at her, there's certain anatomic things you see, she's got some deficiency, we have breast tissue along the upper portion of her breast. She's got a well-defined crease at the bottom of the breast.
In general, she is just lacking volume. Diffusely, but predominantly along the inner and the, the upper portion of the breast. So I'd want to find out, you know, she wants to be larger. What does that mean in Texas? That might mean something different than I might in San Diego. And I might mean something different than it does in New York City.
But things that we'll do is we will, you know, do some basic measurements. Every time you see a plastic surgeon, you'll see them pull out a tape measure and they'll measure things to look for degrees of droopiness. And especially, it doesn't seem to have much in the way of droopiness, what we call ptosis.
We'll do things to measure the width of the breast. That'll help us determine what size implant we can put in the patient. We'll have a conversation about putting the implant in front of the muscle or behind the muscle. Generally for most of us, the default position is to put it behind the muscle because it can do a better job of camouflaging, the upper portion of the implant.
It can do a better job of helping you allow, to prevent capsular contracture. It can do a better job with allowing you to yeah. better mammograms in the future. And then once I sort of have that basic information, I want to find out a little bit more about her aesthetic goals. if she is leaning towards a very natural, relatively subtle enhancement, it'll steer me towards one type of implant, which I won't say everything.
I'll leave some stuff for Dr. Pacella to talk about. If she wants a round or bigger look, we might, we might try a different style. So that's, those are the initial thoughts that go through my head. When I see a patient.
Dr. Salvatore Pacella: [00:04:25] Yeah, and those are, those are excellent comments and excellent evaluation. just expand on that.
I, you know, I oftentimes spend a bit of time at the initial consultation talking about breast implants after the fact kind of what to expect afterwards, particularly throughout a patient's lifetime and, and a couple of topics commonly come up. Number one is. Do I, you know, I don't necessarily want to be in a position where I want to change these things out every 10 years, patients often have this sort of misconception that it's, you know, at 10 years you've got to change them out like a, you know, like a battery or a set of tires. And that's a common myth with, that I think was propagated by a lot of the implant companies and a lot of places, surgeons wanting to get patients to come back for for more augmentations at 10 and 20 years.
And you know, in today's day and age with all three, all four, implant companies that are involved in the United States or that sell products in the United States, we're seeing a much heartier construct of implants, you know, exceptionally low rupture rate in some instances, less than 5% of the implants lifetime.
And so that's really important. I think for patients to understand is just because you have an implant doesn't necessarily mean that at 10 years you have to change it out. Now I do counsel patients and tell them that the longer these implants are in. There's a, there's a significantly higher chance that there will be some issue with them.
So if you're a young patient at age 22, getting a breast implant, chances are at one or two times in your lifetime, there's going to be a need to do a replacement or some sort of revision. And, and I think many patients tell me as well, you know, when I'm. When I'm 65, I'm 22 now, when I'm 65, I, I'm not going to care what my breasts look like.
So I'll just take 'em out and it won't be that big of it, but believe me, and I'm sure you too will reiterate this as at 65, you're going to care.
Dr. Sam Jejurikar: [00:06:25] Exactly more strongly. I totally agree.
Dr. Salvatore Pacella: [00:06:32] So the lesson here is that implants are a lifetime. Thing. there's no going back to just simply taking them out at 20 or 30 years down the track. The reason being is, it's twofold. the act of putting in an implant will stretch out the tissue. It creates an anatomic space in the body that can't necessarily be filled up back with your normal tissue.
The second issue is that tissue around the breast will stretch over time. So just like a normal breast would age. And that's oftentimes impossible, very difficult, if not impossible to correct without placing another implant later in the future.
Dr. Sam Rhee: [00:07:12] I think, there it's, for me, these initial patient consultations can be challenging because there's so much information that has to be related to a patient.
And Sam touched on many aspects of it and so did Sal. And so it's sometimes not so easy for a patient to process everything, especially when their only goal is I want my breasts to be larger. And, to, to know all of the things that you, you two have mentioned, it does take a little bit of time to process that.
I think, one of the things that was a takeaway, I think, I don't remember who said that at Michigan, but it was always, these are, you know, these are not, implants that you're going to have for the rest of your life. At some point, you're going to need another operation, probably if you're, you know, even if you're young, or old, you know, you may need an upsize downsize, exchange, you know, deal with scar tissue, what have you, leak. So I always tell patients, don't expect that if you have implants put in that you will never have to worry about them again, there is there's care involved, just like there is anything that's manmade. I am interested in hearing, I know Sam, how you to determine. what volume is appropriate for a patient?
Like you said, there are major regional variations, and there's also a way of trying to find out what the patient wants. And I know Sam, you do digital imaging and I'm interested in hearing about that as well as, what else, you guys do for that?
Dr. Sam Jejurikar: [00:08:41] Yeah, I'm, I'm, I'm a big proponent of, Three D imaging. I use Crisalix software on my practice. I don't think it's foolproof by any stretch of the imagination, but it's an excellent communication tool, what patients. So what I would typically do for a patient that I'm seeing for a consult like this, and this is happening via telemedicine these days, this is happening. Even in person in the office, we'll do some basic measurements and I'll try to get an idea of what aesthetic she's looking for. Does she want to look natural? Everybody says they want to look natural when they come in. Not everybody really means that, how big of an enhancement does she want? How much roundness she want on the top of the breast.
And then, based off of the diameter of their - of the patient's breast, I will make some initial implant selections and we'll adjust the implant profile. So patients will come in with pictures of patients that they like, and they'll, they'll see it. Different names like moderate profile, high profile, moderate plus full profile.
And they don't really quite understand what it is, what well basically is, is a word way to look at the relative with, to the projection of an implant, meaning a high profile implants, a relatively narrow rounder implant. That's going to give you in general, a faker look more roundness on the top, which some patients really want the lower sounding the adjective is so moderate sounds lower than high that the, The the less, the implant will stick out. The more natural slope you'll have on the top of the breast.
So if this patient were to tell me, I want to have a natural appearing breast and she genuinely wants that and she wants to be, you know, one, one and a half cup sizes bigger, I might start showing her some implants that are moderate profile implants with three D imaging, to get a sense as to what she's looking at. if we agree on one that she actually likes, I'll make sure on the day of surgery, I'll actually have that implant. Plus some others there as well.
Just, just in case the measurements that we came up with three D imaging aren't. accurate, which oftentimes they are not particularly when the patients are doing their own measurements at home. but that, that's how my basic approach would be. You know, it's a lot of back and forth, a lot of communication, a lot of initial, a lot of additional communication, even after the initial consultation, when there's some buyers remorse about the size they chose.
Dr. Salvatore Pacella: [00:10:58] Right. I think, You know, a phrase I, I really believe when it comes to sizing for breast augmentation is a, is a picture is worth a thousand words. And, you know, I, if you, you guys use the, three D imaging software, unfortunately we, we don't use that in our practice. and I haven't found it as predictive as just simply asking patients to bring in some examples of photographs and when, and when I meet them again for the second time for the preoperative examination, I asked them to bring in photographs from not necessarily from breast augmentations before and after that they may find on the internet. Those are helpful, but pictures of, of patients or, or, or women it just in popular media.
So for example, in, you know, a swimsuit magazine or a swimsuit ad, and what that's really important for me to understand is the upper profile of the breast. all of these breasts look different in a bra versus without a bra and, and patients, I think sometimes don't necessarily, can't necessarily articulate that.
And so when I have that situation very frequently is when a patient comes in and says, you know, I want a natural look. And then I asked them to bring in photographs and they have a huge projection implant that basically they can, they can put their White Claw on top of, on top of it, okay. That's a very high profile implant that is not necessarily going to give you a, a moderate slope or a natural look.
So, so bringing those pictures to the preoperative appointment is, is critical for me and, and the patient's sizing. and I, you know, and I bring those in the operating room. I hang them up in the operating room. I try to match it one for one as much as I can. I think in general, when it comes to ordering the size of the implant, I, I try to get patients to be a little bit flexible on the size.
Many times patients will come in and say, well, you know, I saw this online, this woman has a 325 moderate plus I absolutely want that implant. Well, that, that may not really be a great size implant for you at every, every patient is different. Every time size of breast, both the projection and the, and the width are different.
And so I usually try to get a range of implants within about 50, 50 CCS or so, so, That way we have the ability to go up or down based on the particular size and going back to Sam's Jersey Sam's patient here. when I look at this patient here, the left breast looks just a smidge smaller than the, than the right breast to me, and you know, that that's something that is going to. When you put the implant sizer in, in the operating room, that's something you're going to necessarily notice. So I want the flexibility to add 25 or 50 CCS onto that left side. If I, if I want it to. And that's, that's oftentimes not that easy without having a variance of sizes,
Dr. Sam Rhee: [00:13:52] Listening to both of you guys, two things strike me.
One is there's a variety of ways to understand what the patient wants. And, it's like surgery. We have all sorts of different tools. It doesn't necessarily matter what that tool is. And we're all good with our tools. So whatever we, we like, we, we use, whether it be Crisalix, digital imaging, whether it be assessing, what the patients bring in photograph wise.
I also use sizers, which are these, you know, basically silicone shell type cups that, patients can, test with as well. I feel like all of these things are very good in, and, and the key that the other takeaway I'm getting is is that it's trying to really understand what the patient wants.
And one of the big things is that upper pole fullness, like how big is that breast going to look on the upper part of it? And you know, whether it's white claws, you know, big or natural appearing. That's a good one. I'm going to use that. That is, I think we all realize that is a big aesthetic that we have to, understand what it is that the patient wants, because sometimes the patient does not even realize that until we see their, they see their own imaging or, bring in photographs of themselves or try different things.
What is it that you guys, when patients ask, what are the major risks or concerns? what do you touch on with your patients before breast implant surgery?
Dr. Sam Jejurikar: [00:15:25] I mean, the one that I think we probably all spend the most amount of time talking about is something called capsular contracture. That's the most common, most common complication that you'll see with a breast implant and the instance of it varies, depending on implants and anatomic location, but it's thought to represent a, a low grade bacterial infection or a biofilm basically around the implant. So, we talk about tools that I can do during surgery to try limit the incidents of that happening. you know, we all use a variety of antibiotic concoctions during surgery and iodine ointments to try to diminish, you know, bacteria from the skin, from actually getting into the pocket.
I'm a big fan of something called the Keller funnel, which I'm not sure if you guys use it or not to insert the implant, it allows the no touch implant. There's still a lot of surgeons that don't use it, so that's why I don't, add introduces a small cost, but yeah, I'm shocked by the number of plastic surgeons. I know that still don't use it, but it allows you to do a no touch technique to put it in.
So we'll talk about that. the. That the two ones that people complications that people really want to spend a lot of time talking about and I'm gonna bring them up and then let them to hear Dr. Pacella and your take on this, our breast implant illness and breast implant associated lymphoma. So I'm curious what you guys tell patients about those two, those two risks.
Dr. Salvatore Pacella: [00:16:39] Yeah. So, so to back up a little here, I, I really talk about complications, and in two scenarios, there's the immediate complications from the surgery. And then long-term complications afterwards. And so, you know, and we touch on these very briefly. I often we, we give patients a, a big, large, packet or documentation talking about every specific potential complication in general.
So we, we basically just graze on this and the, in our preop appointment. So. Immediate complications, based on their health. you know, anesthesia is very safe. Obviously it's a short procedure. We're not involved in big major body cavities where there's potential for damaging major deeper structures.
But you know, the most common complication immediately after surgery is the risk of bleeding. And I give patients a percentage is less than 1.5%. If bleeding does occur. And it's a small amount of bleeding. We can often types manage it. So we just compression and ice. but if it's a substantial amount of bleeding, meaning a hematoma and blood is collecting in the pocket, we have to take it back to the operating room and sort of, we talk about the ramification and then onto the long term complications, you, you, you touched on the risk of capsular contracture, and we do go over that. But as far as the two topics of breast implant illness and breast implant associated lymphoma. you know, I do give patients some literature on that. So let me first talk about the, the lymphoma, the lymphoma risk.
We, I really want to highlight that that risk of developing breast implant associated lymphoma is almost exclusively in implants that are textured versus implants that are smooth. and like most surgeons across the country, I've, I've tried to just completely remove textured implants from my practice in order to, to, to mitigate that risk.
The other thing I talk about is there's some data on the specifics are different types of companies based on their, on their type of texturing. And, there is really one company that has been implicated with the highest risk that's the company that has been removed. their texture device has been, they removed from the market.
and I don't actually use that particular company. I use the other two companies. So in general, that's a very low risk that I think patients are willing to accept the, the, the concept of breast and breast implant associated illness is, is a little bit nebulous. you know, unfortunately we don't have a ton of data out there and arguably, silicone breast implants, probably.
The device that has been studied the most out of the FDA for the last 30 years. I mean, we have a tremendous amount of data on, on this topic, but no data set has really implicated or created this, this idea that breast implants cause systemic illness. And, and, and I, I don't necessarily say that that's not real.
I think there is some component to it. but I can also say that many times in my practice when patients have come in and they've said my breast implants are causing X, Y, Z. We've went ahead and taken those implants out. And none of those patients have actually improved their symptoms, which tells me that there's probably some other, you know, inciting cause to, you know, autoimmune disease. These are rheumatologic disease, et cetera. So it, it it's, it's, it's a very vague thing. I think we don't necessarily have a huge handle on as surgeons.
Dr. Sam Jejurikar: [00:20:10] So when you say those patients didn't get better, you're doing implant removal, en bloc capsulectomy.
Dr. Salvatore Pacella: [00:20:15] Correct. And no replacement.
Dr. Sam Jejurikar: [00:20:18] What, and what period of time did you follow them?
Dr. Salvatore Pacella: [00:20:21] Usually I follow patients at least, two to three years afterwards, usually every year, just to check a check on them. So, you know, most of these patients have been two, three years out, you know, What has been your experience?
Dr. Sam Jejurikar: [00:20:35] You know, I've seen a lot of women that have, come to me with implant related problems that they have called breast implant illness.
And I think probably. 85 to 90% of the time. It was profound capsular contracture, or malposition issues, or just related to the size of the implant. So, and I, and I, and I think those are legitimate, real implant-based problems that require surgery. There's been about a half, a half, a dozen who genuinely had sort of, autoimmune type of symptoms, food allergies, hair loss, generalized fatigue, arthritis, arthritic type of symptoms who we've taken out their implants, done en bloc capsulectomy and initially not a huge improvement, but over the course of six to 12 months in improvement.
And I've actually seen in the women that I was pretty convinced had breast implant illness. I've seen an improvement in all of them. Not complete resolution of symptoms, but improvement. So, but, but you know, it's, but a lot of, you know, there's been a lot of cases where we've, we've done en bloc capsulectomies, and we've done implant removal, but I really think it was more for capsular, you know, grade four, which is the most severe type of capsular contracture and then doing that's a great treatment for that too.
Dr. Salvatore Pacella: [00:21:50] Jersey Sam limit. Let me ask you this. When patients come in and ask you to perform an and block, capsulectomy, what's your discussion with them? What, what do you tell them?
Dr. Sam Rhee: [00:22:02] I mean, I don't do en bloc very often.
Dr. Salvatore Pacella: [00:22:04] I think they're specifically a patient that says, you know, and the reason I ask is that there's a huge, internet push on this topic, the en bloc capsulectomy the idea is that. Somehow there are some humors inside the implant capsule that if, if they are violated during the course of removal, that those are going to increase the patient's symptomatology. So a patient, what I'm curious about is patients that come in and ask specifically, do you do this? And am I going to have this done?
Dr. Sam Rhee: [00:22:40] I have not done an en bloc I think in a very long time. If someone comes in specifically asking for that, I don't think I can ever necessarily guarantee that I'm not going to release evil humors at the time that I do. And, you know, a capsulectomy like that. And, my, my question really is, is I don't really have, I mean, the issue is this breast implant illness is not well-defined, it's a very difficult phenomenon to quantify because we don't have good data on it that that is, extensive in terms of, real research. there's no doubt that we have seen anecdotal cases, but we've also had anecdotal cases for rheumatoid and lupus and other autoimmune diseases associated with breast implants for many years.
And none of the studies have borne that out. How many patients are you seeing that want en bloc capsulectomy and that are demanding that as their only treatment to address their symptoms?
Dr. Salvatore Pacella: [00:23:36] A lot, a lot. And I will say that part of it is because I I'm involved with a - major health system. I take insurance and you know, that that is a, this is usually our reconstructive phenomenon that we, that we see. Texas, Sam me, let me. Can, can you answer that question when someone comes in?
Dr. Sam Jejurikar: [00:23:59] So, that's a, that's a great question because I, I'm also seeing a lot of patients that, that want this done and, I want to be able to do it and everybody that asks it, but it is a difficult thing to do in certain patients. If you have a patient with a severe capsular, contracture and thin beast tissue and a thin upper pole tissue.
It can be technically challenging to do that. And sometimes it is nearly impossible to get it out en bloc. So we'll have a discussion at that point about my desire to perform a complete unblocked capsulectomy and what the alternatives are. If I can't get it out in one piece, I'll stress to them that I will take out all of their kids.
Absolutely. Even if I can do it en bloc and for the people listening en bloc means you're taking out the implant and the entire capsule, the front and the back wall of it out in one piece in a relatively large breasted with natural tissue woman, with a smaller implant for me, technically, that's easier to do than a woman who has a dense capsular contracture on a relative deficiency of, of, of breast tissue.
So if, you know, and like you guys have said the data, there's not a lot of data to suggest that capsulectomy is, or, or to prove that capsulectomy is required to treat. You know, these vague autoimmune diseases. However, there's a lot of people that have very strong feelings on this issue. And so it's my desire to be completely truthful at all times, discuss the, because I have seen surgeons who, are basically crucified on the internet and because, patients will accuse them of not having taken out the entire capsule afterwards.
This is a huge, a huge bone of contention. So someone says, I need you to take out the whole capsule or we have this discussion. I'll take it all out. But I'll be honest about my ability to do it in one piece versus not doing it in one piece.
Dr. Salvatore Pacella: [00:25:47] Right. And you know, there are, there are, unfortunately, you know, this is sort of goes back to marketing and, and, and media in plastic surgery.
And unfortunately there, there have been some surgeons in this country who have really taken advantage of patients, I think. Okay. And created this. This idea that you can only have a, en bloc capsulectomy and you know, to me, it's, it's like a, you know, a, a, a Yeti and a unicorn or mermaid. Those all sound really cool and, you know, feasible to exist in the world.
But in practice, they, they probably don't exist. The surgeons that. Let's say that I only exclusively do en bloc capsulectomy I don't think are being as truthful as, as the rest of the country. This is particularly the case with implants that have, that have been placed sub muscular, you know, it's exceptionally difficult.
At times to take off the back of the capsule on the chest wall. You're talking about right on top of the rib cage. if there's lung tissue that's right below this, and scraping off every little piece of capsule can be near impossible, if not impossible to do it all in one swoop. So I think, you know, the key concepts I think for patients to understand is ideally we do want to do an in block capsulectomy if possible, but oftentimes it's not possible.
And, and the consequences of doing that is you can take an operation that, that requires a scar, this big to one that requires a scar this big, and that's, that's sometimes a very difficult pill for patients to swallow.
Dr. Sam Jejurikar: [00:27:25] Right. I completely agree with that assessment. Yeah, completely.
Dr. Salvatore Pacella: [00:27:29] So we're so let's move on to the results here. I think we're running close to the end of our block here.
Dr. Sam Rhee: [00:27:34] Alright. So the patient opted for, and we didn't get to it, but saline implants, they were high profile and, they were done as a, we commonly do is a sub muscular or partial sub muscular. So dual plane. And, through an inframammary incision, cause you can't see the nipples, so I'd have to tell you that. so it was an incision, right at the base of the chest.
And Sal was right. I did, 380 on the left and 350 on the right. So you, you called it in terms of the asymmetry. and,
Dr. Sam Jejurikar: [00:28:13] Did you do a tummy tuck too, some lipo?
Dr. Sam Rhee: [00:28:15] You know, it was funny cause you told me, remember we talked about this in one of the podcasts, how we don't have like. I was like, Oh, patients that come back for multiple, multiple procedures.
Yeah. And, and you said more of your patients do that then you, I think, and I, she did, she, this was after she actually had her breast aug and then she had a lipo BBL done about a year or two after. And so this was actually after the lipo BBL as well. So this was actually like a two year postop result.
Dr. Sam Jejurikar: [00:28:43] That's great.
Dr. Salvatore Pacella: [00:28:46] It's a great result, Sam. I really think it, you, you really did a couple of things exceptionally well here. Number one is, is just the natural appearance of the implant. And this is our viewers and listeners may not necessarily appreciate this, but too. To get this type of result with a saline implant at two years is exceptional.
And you know, it really has created a lot of good lower pole fullness and good natural slope to the upper pole. This just looks great. No rippling whatsoever that I could see from this, which is sometimes a risk with saline implants. So you really hit that the nail on the head here. The other thing I think that you did exceptionally well is the cleavage area, particularly at the lower pole, on the inner surface of each breast. If you look at the right breast and the preoperative photograph, You can see that, you know, maybe it's just the shadow, but many times the breast has a little bit of a cone, like appearance to it in that, that you could see that clearly on this gal, on both sides, but more particularly on the right side.
So she doesn't really have a ton of extra breast tissue on the middle of the breast, down at the lower portion right here. And you just masterfully filled that in with your implant, which looks phenomenal. So really, really great job.
Dr. Sam Rhee: [00:30:03] Thank you. I appreciate it.
Dr. Sam Jejurikar: [00:30:04] Kudos, wonderful result. Really I echo everything Sal said.
Dr. Sam Rhee: [00:30:09] That was great. I appreciate all the kind words on that one. I know you guys, have, I think it's interesting to see how many regional variations there are, in terms of what are the most average size implants that you typically place in your practice?
Dr. Sam Jejurikar: [00:30:25] I mean, there's a, there's a huge range at this point. It ranges, in my practice from 200 CCS to 800 CCS. it's all over the place, but it's not the same stereotype of Texas that always has previously existed. And everything is not always bigger in Texas, but sometimes it is. Yeah.
Dr. Salvatore Pacella: [00:30:45] I, I would say that, you know, in general, the the average on the bell curve is probably in the range of 350 to 450 that I would, I would perform.
Dr. Sam Rhee: [00:30:54] Yeah, that sounds similar to me too.
Dr. Salvatore Pacella: [00:30:57] You know, just, just to back up here for our viewers on that last result, You know, all three of us have trained together or we're all very, very close friends and we all, I think have an artful and masterful way of telling each other that we're, we're full of doggy do-do.
So we're not, we're not three people that would shy away from telling each other, Hey, that's a terrible result or you don't, you're not, you, you know, you're just completely off base here. We all, all three of us have comfort in telling each other that. So for us to, to really say that, you know, the results look fantastic.
I mean, we're, we're, this is an honest, we're not just trying to pat each other's back. You're awesome. No, no, no. You're awesome. You know, so it's. this, these types of results, I think are very difficult to achieve. And, and, and I'm, I'm honored to be in the, in the broadcast studio with these two jokers,
Dr. Sam Jejurikar: [00:31:52] Well said, Dr. Pacella as always.
Dr. Sam Rhee: [00:31:54] Yeah, with that. Thank you so much, Sal. Thank you, Sam. Hope you have a great Sunday. Enjoy
Dr. Sam Jejurikar: [00:31:59] Take care of gentlemen. Take care.